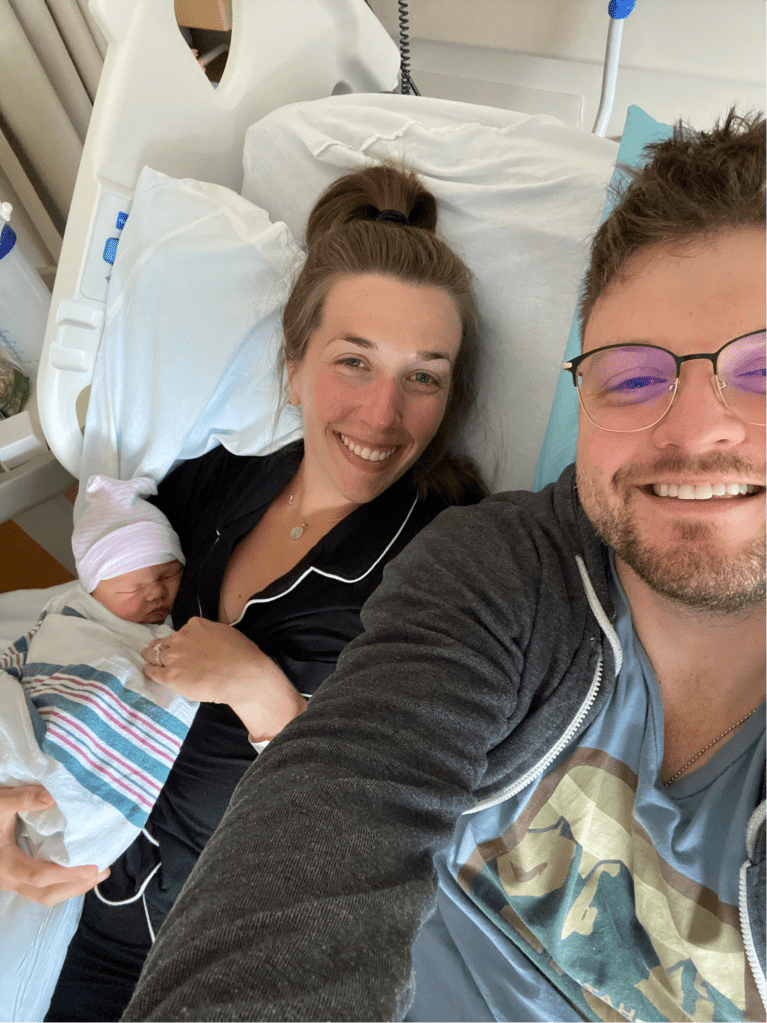
Born 6/21 at 11:45 am
7 lbs 13 oz, 20.5 in long
Our birth story begins on the evening of Thursday, June 19th. I was 38 weeks and 6 days gestation and had been off of work for the week in preparation for the delivery. I remember feeling that day like I was finally both physically and emotionally prepared for the birth of our baby. I had spent a lot of the afternoon on the birth ball doing hip circles and bouncing on the ball. I also did a mini version of the Miles Circuit that afternoon. We had a very normal evening at home, but when I went to use the restroom before we went to sleep, I noticed a very slight brownish/pink tinge to my cervical mucus. I thought to myself that this might be bloody show, but convinced myself it was probably nothing significant. However, when I went to the restroom again that evening, the mucus was much more obviously bloody show. I knew after seeing this that my labor would likely be imminent. I warned my doula, Lindsay Neal, that evening about my symptoms and I tried my best to get some good rest, but my sleep was fitful from the anticipation of the impending labor.
I awoke the morning of June 20th around 5:45 am with what seemed to be relatively consistent contractions. They were very mild, but occurred at regular 4-5 minute intervals, lasting anywhere from 30-60 seconds. I worked hard to relax my body as best as possible and allow the labor to progress. The bloody show continued throughout the morning. My husband and I had plans to get pedicures that weekend in preparation for the birth. This was my only request prior to delivery because I wanted at least one part of my body to feel fresh/pretty in the postpartum period. Given my contractions were still very mild, we decided we’d still try to get pedicures that morning. We had a visit from a family friend that morning around 9am, which was a nice distraction from the surges, and then we headed to get pedicures around 10:30 at a local nail shop in TR. It was an awesome way to pass the time in early labor and release some oxytocin. I remember feeling like it was a fun secret that no one could tell that I was in labor. The man doing my pedicure even asked “When is your baby due?”, and I simply replied that I was due in a week (meanwhile I am actively timing my contractions in the pedicure chair). The contractions were still very manageable after the pedicures were complete, so we decided to let the oxytocin keep flowing and we went to lunch at TReehouse Cafe, one of our favorite local spots. It really was a sweet time spent with my husband.
After lunch, we headed back home and I tidied up the house and finished some laundry. My husband was wrapping up some work duties, as he had to reschedule his patients for the upcoming week for paternity leave. My surges began to feel somewhat more intense around this time but I was still able to mostly talk through them. They were now occurring closer to every 3-4 minutes, lasting at least a minute. I felt them mostly in both of my hips as a very intense pressure-like sensation. After about an hour of this, I called the Greenville Midwifery Care call line around 2:30pm to warn them and get their advice about the best next steps. I reviewed with midwife Barbara the timing of my contractions and discussed that I had hoped to labor at home as long as possible to provide myself with the best opportunity for success with an unmedicated birth. Unfortunately, I had tested positive for group B Strep at my 37 week visit, so I had elected to have the IV penicillin during delivery. This meant that I needed to try to time my arrival to the hospital at least 4 hours prior to delivery in order to get the two recommended doses of penicillin before the birth. Knowing I could still talk through my contractions, Barbara felt that I was still safe to stay at home for a bit longer and encouraged me to go for a walk. She asked that I call back when I could no longer talk through my contractions consistently for about an hour. Around this time, I began to feel like I needed my husband’s support and asked that he quickly wrap up his work responsibilities. We went on a short walk around the neighborhood around 3 or 3:30 pm and I would have to stop to breathe when the contractions occurred, no longer able to really talk through them. It was very hot that afternoon, somewhere in the 90 degree F range, so we decided to keep the walk brief and conserve my energy. My husband, seeing a shift in my behavior, began to feel like we might need more support from our doula at that time, so he reached out to her and she began to head our way with an ETA of around 5 pm. I also gave Barbara a call back at that time, and given the contractions had strengthened and remained consistent since our last call, she recommended that we come be checked in triage to see if I should be admitted and start the IV antibiotics. She said at the time that it was a possibility that I might be turned away if I was not in active labor, and in that case they would have me walk around the hospital a bit more. We headed to the hospital around 4:45 pm and had our doula, Lindsay, meet us at GMH instead.
The car ride was not exactly comfortable for me but was not nearly as intense as I had mentally prepared myself for. While in the car, my husband began to play the birth playlist I had carefully compiled in the months prior. It was filled with relaxed/beautiful songs that we both already had sentimental attachment to, but wow – we had no idea how meaningful these songs would become in the wake of the delivery. I immediately began to cry as the music played, feeling so many mixed emotions about the journey ahead. I was grieving the life we were leaving behind, while also feeling anxious anticipation at the arrival of our first baby.
We arrived at GMH around 5:15 pm and met Lindsay in the parking lot. I was still in good spirits at the time and was chatty/pleasant in between contractions. Unbeknownst to me, Lindsay was concerned after she saw how composed I was that I was likely still in early labor and that they would not admit me. We walked up to triage, having to stop a time or two in the hallway for a contraction. My husband would do hip squeezes for me through the height of the surge. On arrival to triage, they did a cervical exam to assess dilation. I had asked to not be told how dilated I was, so as to not get discouraged by the number. Barbara examined me and said “hmm I think we can admit you!” She told my doula and husband about my cervical exam in private, and I later found out that I was dilated 5 cm at the time.
They got me settled in my L&D room and I continued to labor around the room for the next 2-3 hours. I was given my first dose of penicillin on arrival, with plans for the next dose at a 4 hour interval. The baby was laying in the ROA/ROT position, so my doula suggested that I try to do the full Miles Circuit to see if he would move toward the left side of my uterus for optimal delivery position. I held each of the three positions for 30 minutes. This was not particularly comfortable and I was really having to focus on my breathing to move through each surge. My husband continued to do hip squeezes in any position where it was possible, and Lindsay helped relax me by doing the jiggle in between contractions. I also began using some labor combs at this time, which I did find were somewhat helpful in redirecting the intense sensations.
In the interval, there was a shift change and midwife Maureen started her night shift. I thought for sure at that time that she would be the one to deliver me sometime in the next 12 hours, but spoiler alert she was not. Around 8-8:30 pm, I was beginning to feel like I’d like to try getting in the tub. Maureen suggested I have a cervical check prior to getting in the tub to ensure I had progressed enough and was not going to stall my labor. I agreed to be checked but again requested to not be told about my dilation. She checked me and said I had progressed enough to get in the tub (I was apparently about 7 cm with a bulging bag of waters), so I entered the tub around 9:15-9:30 pm. I continued to labor in the tub for the next 2.5 hours and received my second dose of penicillin during that time. I remember my nurse saying, “This should be your last dose. I think we will have a baby before the next one!” Again, spoiler alert it would not be my last dose – I would continue to receive doses every 4 hours for the remainder of my labor. My contractions did slow somewhat while I was in the tub, occurring around every 6-8 minutes on average at times. However, they continued to intensify, and I was very grateful for the respite in between contractions to compose myself. I started to vocalize through contractions, and I wanted my husband to be right next to me at all times. I would start to panic if he needed to leave to use the restroom, or get a drink/snack, and would beg him to move quickly to get back to me by the next surge. I would squeeze his hands through each contraction and focus on steady breathing/vocalizing and relaxing the remainder of my body. He mirrored any breathing/sounds I was making for the majority of my labor, which really centered me and kept me more relaxed.
Sometime toward the end of my time in the tub, likely around 11pm or 12 am, I began to slightly bear down with contractions and developed the shakes. I felt very encouraged because I knew that this typically indicated transition and/or impending delivery. After about 2.5 hours in the tub, the nurse/midwife encouraged me to exit the tub and change positions to help encourage the baby to descend. It was around this time that I began to feel the physical exhaustion start to kick in – but I was still hopeful that the end was in sight, which sustained me through the intensity of the labor. I would often fall asleep for a brief time in between contractions. Lindsay was amazing at reminding me to eat/drink as often as possible in labor, and I am so glad she did. I fear I would have run out of energy had I not complied with her recommendations. I labored standing up, on the birth stool, and briefly on the toilet – all the while continuing to involuntarily bear down through contractions. After laboring outside of the tub for about two hours, I then entered the tub again around 2:15 am. I think my care team was pretty convinced I was going to deliver during my time in the tub, and the nurses even prepared the birth supplies at one point during that two hour period back in the tub. However, again nothing seemed to progress. I exited the tub again around 4:45 am.
My amniotic sac had remained intact for the whole labor and I was beginning to feel more discouraged at the lack of progress, although I did not vocalize this discouragement for some time. I asked Maureen around that time when it might be appropriate to consider rupturing my membranes, as I was concerned the bulging bag might be preventing progression. She agreed that it would be appropriate to check me again and see how things were looking. I was 100% effaced, but she could feel a small cervical lip that was remaining. She also noted that his head was asynclitic (malpositioned) and she was concerned that this might be the main factor that was inhibiting progression. She strongly encouraged me to again do the first two positions of the Miles Circuit for 30 minutes each to see if we could get his head to adjust, with the plan to break my water if things looked promising after the Miles Circuit. I was very unamused by this suggestion as the intensity of the Miles Circuit at this stage in labor did not sound bearable, but I was willing to do anything I had to do to get our baby out safely/quickly. After an hour of profoundly intense contractions in the Miles Circuit, Maureen returned and re-examined me. She was unable to confidently tell if the head had fully adjusted, but agreed that breaking the water would be the best next step and would hopefully expedite the rest of the labor. She ruptured my membranes at the end of her shift at 7am. The fluid was meconium stained, so I was then unable to return to the tub and was placed on continuous fetal monitoring moving forward.
After rupturing my membranes, the shift changed again and midwife Miranda started her shift. She and Lindsay encouraged me to continue shifting positions with every few contractions, including laboring forward/backward on the toilet. This continued for several hours with no progress, despite the increased intensity and frequency of contractions after the rupture of membranes. Around 9 am, we requested that Miranda check me again to see what progress was being made. The baby’s head was very low at that time, but she again noticed the very thin strip of cervical lip that remained on one side of the cervix. She recommended trying to manually move the cervical lip during a contraction to eliminate that barrier for the head to move down. This was also one of the more intense sensations of the entire labor, as my body was very strongly bearing down with each contraction at this time. Miranda mentioned she could feel the baby’s head at a very low station and felt that the baby was very close to coming out, I just needed to focus on pushing. At this point, Miranda put on sterile gloves and waited expectantly at the bottom of the bed as she and the nursing team instructed me to push as hard as I could. I tried pushing through several contractions on my side in the bed without any notable progress, so I then began to move around to several other positions to push – in the bed on all fours, standing/squatting while pulling on a rebozo. This continued for almost two hours with no observable change. My body was so exhausted, I could barely hold up my weight in a squat to push for the duration of a contraction. Laboring on the toilet was one of the most intense positions during the whole labor. I remember my husband checking in with me while laboring on the toilet and asking how I was doing. I finally admitted out loud that I was starting to feel discouraged. At this time, my husband began to become more concerned that I would run out of energy if progress was not made quickly. For this reason, and the fact that we were expecting baby to come shortly after the last cervical exam, we requested to be checked again to see if any progress had been made after almost two hours of intense pushing.
Miranda checked my cervix again around 10:45 am while I was standing up beside the bed and confirmed no progress had been made. At this time, she made the suggestion to try getting back in the bed again to push. This recommendation was contrary to what most midwives typically would recommend, but she felt I might benefit from more directed efforts at pushing and getting some leverage by pulling my legs back and curling over my abdomen to push. I was instructed to push as hard as I could while the nurse or my husband would count to 10, at which point I would take a breath and continue again. Most contractions lasted for four counts of 10.
Finally, slowly with each push, they began to see the head emerge. As the head was crowning, his heart rate began to decelerate into the 90s in between contractions and Miranda urged me to push as hard as I could with the next contraction to get him out. I had legitimate concerns that I might not have the energy to fully push his head out due to my significant exhaustion, but thankfully I had just enough left in the tank. Two contractions and a few pushes later, Shepherd Charles was born at 11:45 am. The song “I Can Never Be Without You Anymore” by The Secret Sisters played in the background in his first moments of life – truly the most perfect song to enter the world to.

I will never forget the incredible relief I felt as he exited my body and cried for the first time shortly thereafter. It was truly the most beautiful, profound moment of my life. And it was the most intimate journey with my husband over my 30 hour labor – I have never loved or appreciated him more. There is no doubt in my mind that I could not have done it without the support of my doula, in addition to my unwavering husband. Attending Julie’s birth class also provided me with so many helpful tools to endure such a long, challenging labor. I am so thankful for a team of midwives and nurses that trusted in my body and never once suggested or demanded any extreme interventions that were not medically necessary. We had the dream team (actually, several shifts of dream teams) and they were a critical part in making our birth story possible.